Chronic Fatigue Syndrome (CFS/ME): A Guide to Symptoms, Root Causes, and Herbal Remedies
a compassionate look at this complex condition, the science behind it, and how herbs like cordyceps and ginseng may help
Fatigue is something we all experience—after a long day, after a night of poor sleep, after pushing ourselves too hard. But the kind of fatigue that comes with Chronic Fatigue Syndrome, or Myalgic Encephalomyelitis (CFS/ME), is something else entirely. It’s not a tiredness that resolves with rest. It’s a deep, cellular depletion that can make the most basic tasks feel impossible.
As someone who lives with this condition, I want to speak honestly about what it feels like and why it’s so often misunderstood. CFS isn’t just about needing to nap. It’s about feeling like your body has been unplugged from its power source. Even the smallest exertion can lead to a full crash, with days of recovery. You cancel plans, retreat to bed, and wonder why things that seem easy for others leave you feeling like you’ve been hit by a truck. It's not for lack of motivation or willpower. It’s because your body isn’t working the way it used to, and you can’t force your way through that.
This condition affects an estimated two million people in the U.S., yet most go years without a diagnosis or even basic understanding. It was first documented during a public health investigation in Los Angeles in 1934, and nearly a century later, it remains under-recognized and often minimized. Medical education rarely touches it. Many providers still frame it as psychological rather than biological, which only adds to the frustration and invalidation people experience.
But this isn’t a mindset issue. It’s a physiological condition with clear, measurable changes in the body. Research has identified altered immune function, changes in T-cell and natural killer cell activity, elevated inflammatory cytokines, hormonal disruption, and sometimes even autoantibodies. A viral trigger has been proposed, but no single infectious agent has been confirmed.
All of this paints a picture of a body caught in a feedback loop of dysfunction: exhausted, inflamed, and struggling to regulate itself. And while conventional medicine continues to grapple with how to define and treat this condition, many of us have turned to integrative approaches that offer something the system so often withholds: support, validation, and a sense of hope.
Herbal medicine isn’t a cure, but it can help soften the edges of this experience. It offers tools to nourish the nervous system, support energy production, and calm the immune response. Most importantly, it reminds us that healing doesn’t always come in the form of a fix. Sometimes it arrives quietly—in the form of care, gentleness, and the slow rebuilding of trust between body and self.

Exploring the Biology Behind Chronic Fatigue Syndrome
While the exact cause of CFS/ME is still unknown, research has uncovered several patterns that point to dysfunction across multiple systems in the body. It’s not just about low energy. It’s about immune imbalance, disrupted stress responses, potential mitochondrial damage, and a nervous system that struggles to regulate itself.
No single theory explains every case, but the bigger picture helps us begin to understand what’s happening beneath the fatigue.
The Immune Connection
Many cases of CFS begin abruptly after a viral illness, which led researchers to suspect a lingering or dysregulated immune response. Viruses like Epstein-Barr, human herpesvirus 6, and Coxsackie have all been investigated. So far, no single pathogen has been identified as the cause, but immune abnormalities are a consistent finding.
One of the most well-documented is a drop in natural killer (NK) cell activity. NK cells are responsible for eliminating infected or dysfunctional cells, and in many CFS patients, they don’t work as efficiently. The lower the activity, the more severe the symptoms tend to be. Other changes show up in T-cells and immune cell receptors, suggesting the immune system is both overactive in some places and under-responsive in others.
People with atopic conditions—such as allergies, asthma, or eczema—may also have a higher risk of developing CFS, possibly due to immune sensitization.
Energy Breakdown: The Mitochondria
Mitochondria are often described as the “powerhouses” of our cells. I know those of us in the States have had that drilled into our brains during high school science classes.
They convert nutrients into usable energy. In CFS, research has shown possible disruptions in mitochondrial function. This could mean cells are producing less energy or generating more waste products like reactive oxygen species, which can further damage tissues. While this area is still developing, it offers a compelling explanation for the deep, unrelenting fatigue that defines the illness.
My next deep dive will be on the topic of mitochondrial dysfunction.
Mitochrondria
The Brain, Hormones, and the Stress System
The stress response system—also known as the hypothalamic-pituitary-adrenal (HPA) axis—plays a central role in how we respond to physical and emotional stress. In CFS, cortisol levels are often lower than average, though not always low enough to qualify as adrenal insufficiency. This subtle deficiency can affect energy, inflammation, and recovery from stress.
At the same time, the sympathetic nervous system (the “fight or flight” branch) is often overactive. This imbalance may explain symptoms like heart palpitations, dizziness upon standing, and poor temperature regulation. So, while one side of the stress system is under-functioning, the other is overstimulated and leaving the body in a constant state of tension. (Note: POTS is very similar to this list of symptoms. In my experience, chronic fatigue and POTS tend to go hand in hand. If you’re reading this and thinking that this sounds familiar, you’re definitely not off!)
Neuroimaging studies have also shown differences in brain activity, blood flow, and structure. Though these findings are still being understood, they reinforce what patients have long known…that this is a neurological illness.
Behavior, Personality, and the Limits of Psychological Models
Some theories suggest that behavioral patterns—like perfectionism or high achievement drive—may play a role in how the illness develops or lingers. The idea is that some people push through early symptoms, leading to deeper exhaustion, then interpret that exhaustion as needing more rest, creating a self-perpetuating cycle.
While this model may explain part of the picture for some, it doesn’t account for the consistent physiological findings. It also doesn’t sit well with many patients, and for good reason. Psychological theories may help contextualize how someone copes, but they’re not the whole story.
Hormone Transport and Genetic Factors
It’s not just how much cortisol your body makes—it’s also how it’s carried. Cortisol binds to a protein called corticosteroid-binding globulin (CBG). In rare cases, genetic mutations in the CBG gene reduce binding efficiency, which may result in lower available cortisol in the body. These mutations haven’t been consistently found in people with CFS, but they offer one more piece of the puzzle in understanding hormone dynamics.
What Hormone Testing Shows
Many people with CFS have lower cortisol levels on saliva or urine tests, but standard blood testing doesn’t always catch these changes. DHEA and other adrenal hormones are often low as well. Results from stimulation testing, such as the ACTH test, vary widely between individuals.
Corticosteroid treatment has not proven consistently helpful and often carries risks. Even low-dose hydrocortisone can suppress adrenal function over time. For that reason, it’s not considered a safe or effective long-term treatment.
A Note on Long COVID
Since the pandemic, many people have reported lingering symptoms long after their initial COVID-19 infection cleared. Fatigue, brain fog, breathlessness, post-exertional crashes, and strange new sensitivities have become part of daily life for thousands. While Long COVID and Chronic Fatigue Syndrome (CFS/ME) are not identical, they do share key features, especially when symptoms persist for more than six months.
In fact, some people with Long COVID may eventually meet the criteria for CFS. Post-exertional malaise, unrefreshing sleep, cognitive dysfunction, and autonomic symptoms like dizziness or heart palpitations are common in both conditions. Because the mechanisms behind them often overlap, such as immune dysfunction, mitochondrial issues, and nervous system dysregulation, the care strategies that help one may also support the other.
Within my own herbal practice, I’ve seen a growing number of clients dealing with post-viral symptoms that don’t fit neatly into one diagnostic box. One person may have been told it’s Long COVID. Another suspects CFS or fibromyalgia. Someone else might be navigating MCAS, POTS, or an autoimmune condition. It gets incredibly confusing and even more exhausting.
If you’ve found yourself asking, “Why does it sound like I have everything?” you’re not alone. That question is valid. These syndromes don’t always follow a linear path. They blend into one another, shift from week to week, and often leave people feeling dismissed or overlooked by a medical system that struggles with complexity.
This is exactly where herbalism can shine. Not by offering a cure, but by gently supporting the body as a whole. Whether you're recovering from a known virus or navigating a long-standing fatigue condition without a name, there are ways to replenish your energy, rebuild resilience, and begin to feel like yourself again.
Why Getting a Name for This Condition Is So Complicated
Before diving into herbal support, I want to pause and talk about the diagnosis itself—because it’s not straightforward. And if you’ve ever felt confused, dismissed, or frustrated trying to understand this condition, you’re not alone.
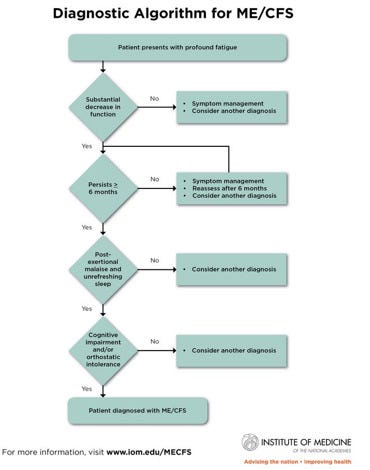
ME/CFS is diagnosed based on symptom patterns, not a definitive test. Diagnosis typically involves ruling out other conditions like sleep apnea, thyroid disorders, anemia, or autoimmune disease. Even with extensive testing, many patients are left in diagnostic limbo
According to the 2000 Clinical Working Case Definition, diagnosis requires:
Fatigue that is new, persistent, and significantly impacts daily life
Post-exertional malaise, where activity leads to a worsening of symptoms
Sleep disturbances, such as non-restorative sleep or reversed sleep rhythms
Pain, including new-onset headaches, joint or muscle aches
Neurological symptoms, such as memory loss, concentration issues, or sensory sensitivity
Symptoms from at least two additional categories, including:
Autonomic symptoms: lightheadedness, POTS, GI disturbances
Neuroendocrine symptoms: temperature regulation issues, stress intolerance
Immune symptoms: sore throats, swollen lymph nodes, flu-like malaise
Symptoms must last at least six months. In children, a shorter duration may be considered. Comorbidities like fibromyalgia, migraines, and IBS are common.
I’m not sharing this so you can diagnose yourself (but if you have an “aha!” moment, might be worth looking into!) I’m sharing it to validate how complex and frustrating this process can be. If you’ve ever felt overwhelmed trying to understand your body, that confusion is real.
Herbal Support for the Fatigued Body
A note before we begin.
In my own experience with chronic fatigue syndrome, I’ve come to realize how misunderstood this condition really is. It’s not just about needing an extra nap (though—yes—daily naps are my norm). It’s the kind of exhaustion that makes motivation vanish, willpower evaporate, and even simple tasks feel monumental. It’s the crash that comes after doing something seemingly normal—like running errands, visiting your nephew, or seeing a few clients—and then spending days in bed wondering why it feels like you were hit by a garbage truck.
People around you may mean well, but the comments can sting. “You’re tired? But you haven’t done anything today.” Or you look at others online who seem to be doing it all without skipping a beat, and you start wondering, Why can’t I keep up?
If that sounds familiar, please hear this: this is not laziness. This is real. And it’s okay to want answers. It’s okay to crave validation from a physician, to hope that someone will simply say, “Yes, this isn’t normal. You’re right.”
As an herbalist, I get it. I understand if herbal medicine isn’t the first route you’re ready to explore. That’s completely fine. Do what feels safe and right for you. Just know that the plants are here, patiently waiting. They don’t ask for perfection. They just meet you where you are.
So if researching your own care feels overwhelming, I got you. Let’s walk through some of the herbs that have been studied, some that come from long traditions, and some that offer gentle, meaningful support for a body that’s deeply, genuinely tired.

What the Research Says, and What Tradition Has Long Known
There’s no magic herb for Chronic Fatigue Syndrome. But herbal medicine can offer support—especially when we take a systems-based, whole-body approach.
In Traditional Chinese Medicine, CFS is often viewed as a mix of deficiency and stagnation. Qi, blood, yin, or yang may be depleted. At the same time, emotional and energetic blockages build. Treatment focuses on nourishing what’s lacking and helping things move again.
Herbs like ginseng (Panax ginseng), dang shen (Codonopsis pilosula), and huang qi (Astragalus mongholicus) are used to tonify qi and rebuild post-illness strength. Others, such as chai hu (Bupleurum falcatum) and zhi qiao (Citrus aurantium), help calm the nervous system and resolve emotional stagnation.
In one small study, a tea made from Astragalus, Angelica gigas, and jujube (Zizyphus jujuba) significantly reduced fatigue, improved sleep, and even helped mood scores over an eight-week period.
A 2023 meta-analysis of 19 trials showed that Chinese herbal formulas outperformed placebo, no treatment, and pharmaceuticals for post-viral fatigue. Some trials even documented improvements in CD4 T-cells and reductions in inflammatory cytokines like IL-6.
Astragalus mongholicus
Adaptogens for Energy and Recovery
Adaptogens help the body regulate its response to stress, which can be especially helpful in CFS, where the stress system is often either overworked or under-responsive. Rhodiola (Rhodiola rosea) is known for its ability to improve focus, stamina, and mental clarity. Schisandra (Schisandra chinensis) supports endurance and helps modulate stress hormones, while Siberian ginseng (Eleutherococcus senticosus) aids physical recovery and builds resilience over time.
Rather than acting as stimulants, adaptogens work by helping cells adapt more efficiently to stress. One of the key mechanisms involves activating Hsp70, a protective protein that guards against energy depletion and oxidative damage. By supporting these internal stress-response systems, adaptogens may help reduce post-exertional crashes and promote more consistent, stable energy.
Cordyceps: A Mushroom for Deep Fatigue
Cordyceps has long been used in traditional Chinese medicine as a restorative tonic, especially for those recovering from long illness or deep burnout. Now, modern research is beginning to catch up—offering compelling insights into why this curious little mushroom might be such a powerful ally for people living with chronic fatigue.
In animal studies, both Cordyceps sinensis and Cordyceps militaris have demonstrated notable antifatigue effects. Mice given Cordyceps extracts swam significantly longer than untreated controls, some by 20 to 24 minutes. But it wasn’t just stamina that improved. Cordyceps appeared to increase ATP production, the cell’s primary energy currency, improve oxygen utilization, and even buffer the body against low-oxygen states. In one study, mice showed up to a 32% boost in heart muscle energy output after just three days of supplementation. That’s a meaningful shift if we’re talking about rebuilding energy at the source, not just masking symptoms.
Cordyceps may also support mood. A concentrated extract showed antidepressant-like effects in mice, thought to influence the brain’s dopamine and norepinephrine systems. It didn’t behave like a stimulant—no hyperactivity, no restlessness—just a gentle shift in baseline mood and motivation.
Another reason Cordyceps stands out is its antioxidant capacity. It helps sweep up the reactive oxygen species produced during exertion, which can trigger or worsen post-exertional malaise. For people with CFS/ME, anything that eases that crash can be a game changer.
Human trials are still limited. Many have used Cordyceps alongside other herbs or compounds, making it difficult to isolate its effects. Trials in healthy individuals often show minimal results, but that may be because Cordyceps isn't about peak performance—it’s about repair. The researchers suggest it may work best when used consistently, over several weeks, especially in those with chronic fatigue or illness.
All of this is why Cordyceps remains a mushroom I keep returning to. It supports mitochondrial energy, balances the stress response, and offers protection against overexertion. It won’t deliver a sudden jolt of energy, and it’s not a magic fix. But it works in the direction of restoration. And for many people walking the slow path of recovery, that’s the kind of medicine that matters most.
Nature's little cheetos
Chronic Fatigue Syndrome isn’t a condition you “push through.”
It’s a complex, whole-body experience that demands patience, nuance, and care. Herbal support won’t cure it, but it can offer something just as meaningful: a way to rebuild, regulate, and reconnect with your body on your own terms.
In my next post, we’ll take a closer look at the mitochondria. What does it really mean to “support” them? Why is mitochondrial health suddenly everywhere in wellness spaces? And what does the research actually say when we move past the buzzwords? I’m excited to explore that with you.
If this piece resonated with you, feel free to like, leave a comment, or share it with someone who might need to read it. And if you haven’t already, subscribe to stay in the loop as we continue unraveling these layered topics together.
Tomorrow’s Library post will include:
A new materia medica on Queen Anne’s Lace
The full “Balancing Hormones” guide
Printable materia medicas for Ginseng, Angelica, Cordyceps, and more
A downloadable Chronic Fatigue Herbal Support PDF, featuring personally tested formulas, lifestyle support, and foundational guidance
Everything will be neatly organized, easy to download, and ready to add to your growing study collection. The Library is available exclusively to paid members of The Buffalo Herbalist.
If you’re navigating chronic fatigue, burnout, or other long-standing health challenges and want personalized guidance, I also offer email-based herbal consultations. These are low-pressure, highly personalized, and perfect for anyone who prefers written support over video calls. If you're interested, feel free to send me a message—I'd be happy to share the booking link, along with all the details. Herbal consultations are just $80 for month of June!
Until then—rest well and be gentle with yourself.
Slow healing is still healing.
With care,
Agy | The Buffalo Herbalist
Bibliography
Lim, W., & Torpy, D. (2023, August 30). Chronic fatigue syndrome. Endotext - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/sites/books/NBK279099/
Sapra, A., & Bhandari, P. (2023, June 21). Chronic fatigue syndrome. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK557676/
Hu, L., Cai, A., Li, B., Li, Z., Liu, J., & Cao, H. (2024). Chinese herbal medicine for post-viral fatigue: A systematic review of randomized controlled trials. PLoS ONE, 19(3), e0300896. https://doi.org/10.1371/journal.pone.0300896
Panossian, A., & Wikman, G. (2009). Evidence-Based Efficacy of Adaptogens in Fatigue, and Molecular Mechanisms Related to their Stress-Protective Activity. Current Clinical Pharmacology, 4(3), 198–219. https://doi.org/10.2174/157488409789375311
Luo, C., Xu, X., Wei, X., Feng, W., Huang, H., Liu, H., Xu, R., Lin, J., Han, L., & Zhang, D. (2019). Natural medicines for the treatment of fatigue: Bioactive components, pharmacology, and mechanisms. Pharmacological Research, 148, 104409. https://doi.org/10.1016/j.phrs.2019.104409
Zhang, Y., Jin, F., Wei, X., Jin, Q., Xie, J., Pan, Y., & Shen, W. (2022). Chinese herbal medicine for the treatment of chronic fatigue syndrome: A systematic review and meta-analysis. Frontiers in Pharmacology, 13. https://doi.org/10.3389/fphar.2022.958005
Lin, B., & Li, S. (2011). Cordyceps as an herbal drug. Herbal Medicine - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK92758/









Hi Agy I didn't finish because I had a question. Can you please clarify how they can be in fight or flight with low cortisol? what hormone drive the sympathetic NS ? Also, my understanding is that CFS is due to dysautonomia many time following a viral infection. I will go back promise. Thanks for writing.
Thank you for this 🙏🏾. I think I may be developing this because my fatigue and chronic pain has gotten increasingly worse. My doctor hasn’t been the most supportive nor helpful, so having this article is a nice companion to ease some of the symptoms while I continue to look for a doctor or specialist. I’m hoping to be able to upgrade to a paid subscription because all of your articles have been so so helpful.