Cravings, Crashes, Brain Fog? Start With Blood Sugar
why glucose regulation matters more than you think, and how to support it naturally
I still remember the week we covered glucose metabolism in biochemistry during medical school—vividly, unfortunately. The pathways, the enzymes, the endless arrows and cycles. It was incredibly daunting, mildly infuriating, and honestly? I still have nightmares about it.
But here’s the thing: for all the complexity, glucose is one of the most essential fuels for the human body. Somewhere along the way, though, I’ve noticed that conversations about “sugar” in the wellness world have gotten... messy. There’s this narrative floating around that any sugar in the brain is harmful. Respectfully, what? That we should be striving for blood sugar levels so low they’re basically flatlined. And yet, I’ve found myself riding the blood sugar rollercoaster more often than I’d like lately—and I know I’m not alone.
So I did what I always do when I’m frustrated and curious: I researched. I pulled together the science on glucose regulation and herbal interventions, and what I found was surprisingly robust. There are herbs that truly support glucose balance, some backed by solid research, others with a long-standing history in traditional medicine.
This week, I’ll be sharing a short series on blood sugar, herbalism, and everything in between. Today’s article covers the physiology and pathophysiology of glucose homeostasis, as well as herbal support for chronic hyperglycemia. Later this week, we’ll get into practical application, individual herb breakdowns, and a full post on stabilizing blood sugar for those of us who swing between highs and lows.
Ultimately, I want readers of this publication to come away with a deeper understanding of how glucose really works in the body, and how herbal medicine can meet us there with nuance, history, and science.
Why Blood Sugar Matters
Let’s get one thing straight: blood sugar isn’t just about avoiding the dreaded crash after a pastry. Glucose is essential. It’s how the body feeds itself, how your brain stays sharp, how your cells stay alive. But like most systems in the body, it works best within a certain range. Too much for too long, and we start to see damage at the cellular level. Too little, and the brain doesn’t function properly. Either way, something’s off.
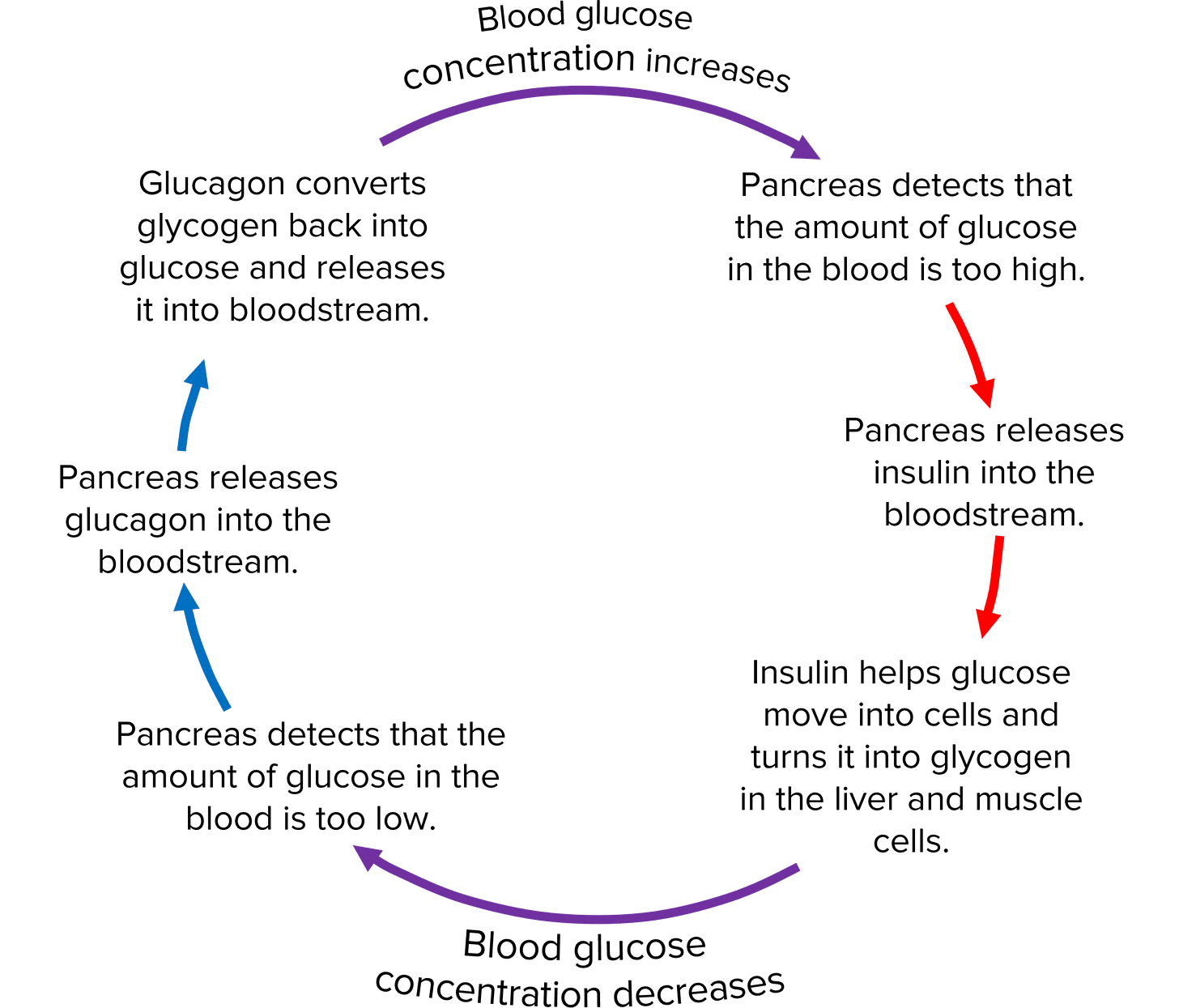
Glucose moves through the bloodstream to reach the cells that need it, and that entire process is kept in check by a tight hormonal feedback loop. The key players are insulin and glucagon, both produced by the pancreas. After a meal, insulin helps shuttle glucose into the cells so it can be used or stored. When you haven’t eaten in a while, glucagon signals the liver to release stored glucose to keep things steady.
Extra glucose gets tucked away as glycogen, mostly in the liver and muscles. Insulin is the signal to store it. Glucagon is the signal to pull it back out. This exchange is happening constantly as your body responds to hunger, energy output, and stress.
When that balance starts slipping—because of processed foods, chronic stress, disrupted sleep, or underlying metabolic issues—the system falters. You might notice:
Fatigue or brain fog after meals
Shakiness or irritability between meals
Increased hunger or sugar cravings
Weight changes that don’t make sense
Inflammation or hormone shifts that don’t respond to surface-level fixes
Blood sugar regulation affects far more than we tend to realize. It’s connected to mood, focus, energy, stress resilience, and how our bodies handle inflammation. It’s not just a blood sugar issue. It’s a whole-body pattern.
And herbs, when chosen thoughtfully, can absolutely help support that balance. But to use them well, we need to understand the terrain first.
How Blood Sugar Is Regulated: A Whole-Body System
The body doesn’t leave blood sugar regulation up to chance. It’s one of the most tightly controlled processes in human physiology, involving constant communication between hormones, organs, and even individual cells. Every time we eat, move, rest, or experience stress, this system adjusts in real time to maintain balance.
The Pancreas: Command Central
At the core of this system is the pancreas. Inside are clusters of hormone-producing cells called the islets of Langerhans, which contain:
Beta (β) cells, releasing insulin when blood sugar rises
Alpha (α) cells, releasing glucagon when blood sugar drops
Insulin and glucagon work in direct opposition to maintain stable glucose levels. After a meal, insulin helps shuttle glucose into cells and signals the liver and muscles to store the excess as glycogen. Between meals, glucagon tells the liver to break down glycogen and release glucose to keep blood sugar steady.
The Liver: Your Metabolic Bank
The liver acts as both a storage site and a backup generator. In energy-rich states, it stores glucose as glycogen in response to insulin. During fasting or physical stress, it breaks down that glycogen or produces new glucose from amino acids and other sources through gluconeogenesis.
It also handles the conversion of other sugars, like fructose and galactose, into glucose. Once processed, glucose is released into the bloodstream and sent wherever it’s needed most.
Muscles and Fat: The Glucose Users
Muscle and fat cells are among the biggest users of glucose, especially after meals. Their ability to absorb glucose depends on a specific protein called GLUT-4. In the absence of insulin, GLUT-4 remains inside the cell. When insulin binds to its receptor, it prompts GLUT-4 to move to the surface, allowing glucose to enter the cell for energy or storage.
This process becomes less efficient in insulin resistance. The signal weakens, GLUT-4 doesn’t move to the membrane, and glucose builds up in the blood instead of entering the cells.
The Other Glucose Transporters
The body uses several glucose transporter proteins, each with its own job:
GLUT-1 supports steady glucose uptake in red blood cells and the brain
GLUT-2 helps the liver and pancreas detect and respond to glucose
GLUT-3 serves the nervous system, with a strong ability to pull in glucose
SGLTs (sodium-glucose transporters) work in the intestines and kidneys, actively absorbing glucose using sodium gradients
Unlike GLUT-4, most of these work independently of insulin. They help ensure that critical tissues like the brain and gut get what they need, regardless of your metabolic state.
Hormones Beyond the Pancreas
Insulin and glucagon aren’t the only hormones involved in glucose regulation. Several others step in depending on your stress levels, activity, and overall metabolic demand:
Cortisol raises blood sugar by promoting glucose production and reducing insulin sensitivity
Epinephrine acts fast during acute stress, helping break down glycogen and release stored fuel
Thyroxine from the thyroid increases glucose absorption and raises overall metabolic rate
Growth hormone and ACTH raise blood sugar through indirect effects on insulin and metabolism
Together, these hormones form a safety net. They keep glucose available during times of need, whether you’re fasting, exercising, or under pressure.
When Blood Sugar Regulation Breaks Down
When the body’s system for managing glucose begins to falter, the effects show up everywhere—not just in lab results. Blood sugar imbalances impact energy, mood, hormone function, inflammation, and long-term metabolic health. And often, the early signs are easy to overlook or chalk up to other issues.
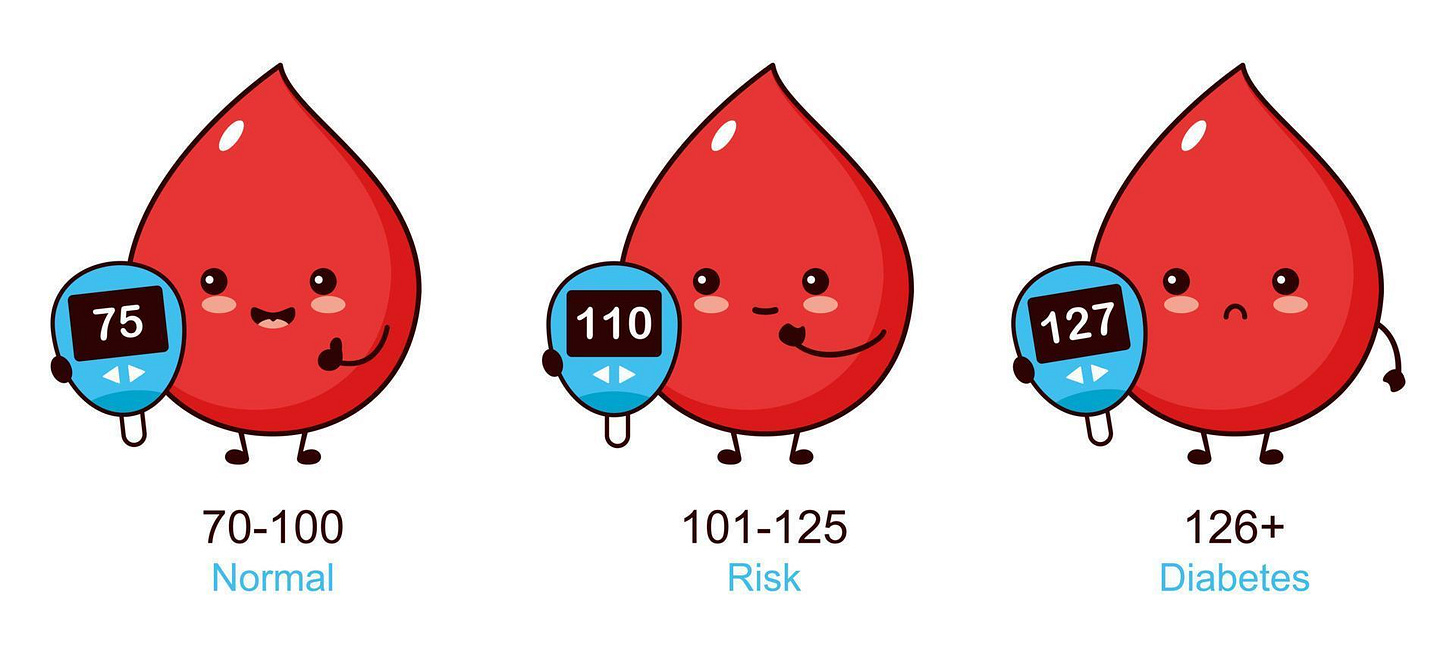
Chronic High Blood Sugar (Hyperglycemia)
Hyperglycemia refers to consistently elevated blood glucose levels. It’s common in Type 2 diabetes and metabolic syndrome, where the body still makes insulin, but the cells stop responding to it. This is called insulin resistance, and it forces the pancreas to work harder to keep blood sugar in check.
Over time, that system becomes strained. Blood glucose remains high, insulin may begin to drop, and cellular damage starts to accumulate. Glucose promotes oxidative stress, leads to glycation (disruption of protein structure), and causes osmotic shifts that can damage nerves and blood vessels.
Symptoms of hyperglycemia can include:
Fatigue or sluggishness
Brain fog or difficulty focusing
Blurry vision
Slow wound healing
Tingling or numbness in the hands and feet
Left untreated, hyperglycemia contributes to long-term complications like cardiovascular disease, kidney dysfunction, and chronic inflammation.
Low Blood Sugar (Hypoglycemia)
On the other end of the spectrum, hypoglycemia happens when blood sugar drops below what the body needs to function well—especially the brain, which relies heavily on glucose. While it often occurs in people using glucose-lowering medications, it can also show up in those with adrenal dysregulation, reactive hypoglycemia, or unstable eating habits.
Common signs of hypoglycemia include:
Shakiness or lightheadedness
Irritability or sudden anxiety
Intense sugar or carb cravings
Sweating or heart palpitations
Headaches, blurred vision, or brain fog
When these symptoms happen regularly, especially in response to meals or stress, it may indicate an underlying regulatory issue that needs attention.
The Blood Sugar Rollercoaster
Many people move between mild highs and lows all day long. A sugar-heavy breakfast followed by a crash. That 3 p.m. energy slump. Waking in the night with a pounding heart. These fluctuations reflect a body struggling to maintain glucose stability, often triggered by inconsistent meals, caffeine, poor sleep, or long-term stress.
The pattern often looks like this: a meal spikes blood sugar, insulin clears it too quickly, and cortisol or adrenaline step in to compensate. Over time, this loop wears down your energy and affects mood, sleep, appetite, and focus.
When the Pattern Goes Deeper
Even in people who haven’t been diagnosed with diabetes, chronic blood sugar imbalance often shows up in other ways. Some of the more common patterns include:
Insulin resistance, often with abdominal weight gain and constant hunger
Metabolic syndrome, a combination of blood sugar dysregulation, high blood pressure, and lipid imbalance
PCOS, frequently driven by insulin excess
Non-alcoholic fatty liver disease, where the liver becomes overloaded with sugar conversion and storage
These conditions often begin subtly, with symptoms like cravings, energy dips, or mood swings. Recognizing them early gives us more room to intervene—especially with herbs that support balance at the root.
The Herbal Approach to Blood Sugar
Before lab work and glucose monitors, people turned to plants. Across cultures and centuries, herbal medicine was used to support symptoms we now associate with blood sugar issues: constant thirst, fatigue, frequent urination, and slow healing. These traditional systems didn’t use modern terminology, but they understood patterns in the body and used herbs to bring things back into balance.
Herbs were never obsolete. They were pushed aside as pharmaceuticals became the dominant model. Yet many of those pharmaceuticals were developed from plants. Metformin, now a first-line drug for Type 2 diabetes, came from a compound found in Galega officinalis, also known as French lilac—an herb with a long-standing reputation for supporting blood sugar regulation.
Medicinal plants contain a wide range of compounds that often work across multiple systems. A single herb might support insulin sensitivity, reduce inflammation, influence gut function, and help regulate carbohydrate metabolism. That kind of complexity makes them particularly well-suited for addressing something as layered as blood sugar imbalance.
More than 1,200 herbs have been used in the treatment of elevated blood sugar, and over 400 of them have been studied for their specific actions. Some protect pancreatic beta cells, some slow the absorption of sugars in the digestive tract, and others improve the way our cells respond to insulin.
As interest in herbal medicine grows, so does the flood of generic advice. Not every supplement is safe, effective, or well-formulated. Which is why it’s important to look at individual herbs and how they actually work in the body, with attention to research, tradition, and context.
Let’s start with one of the most well-known herbs in this space: cinnamon.

Cinnamon: Glucose Regulation and More
Cinnamon isn’t just a warming kitchen spice. It’s also one of the most widely studied herbs for blood sugar regulation. Across multiple clinical trials, cinnamon has shown promising effects in lowering fasting glucose, improving insulin sensitivity, and supporting lipid balance in individuals with Type 2 diabetes and metabolic syndrome.
Several forms of cinnamon exist, but most research has focused on Cinnamomum zeylanicum (Ceylon cinnamon) and Cinnamomum cassia. While both offer blood sugar benefits, Ceylon cinnamon is generally preferred for long-term use due to its lower coumarin content.
Clinical Evidence
In human and animal studies, cinnamon extract has been shown to reduce:
Fasting blood glucose
Post-meal glucose spikes
HbA1c levels over time
Markers of insulin resistance
One clinical trial using a powdered herbal formula—containing cinnamon along with fenugreek, nettle leaf, walnut, and others—demonstrated significant reductions in fasting glucose, postprandial glucose, HbA1c, and insulin resistance over 12 weeks. Cinnamon’s presence in the formula likely played a role in these outcomes, contributing both glycemic and lipid-lowering effects.
How It Works
Cinnamon seems to support blood sugar balance through several overlapping mechanisms. It may help the body respond more efficiently to insulin, making it easier for glucose to move out of the bloodstream and into cells. Some studies suggest that cinnamon encourages the production and movement of GLUT-4, a glucose transporter protein found in muscle and fat tissue. When this transporter is active, blood sugar levels tend to drop more steadily after meals.
The study mentioned earlier found that cinnamon may also help reduce the liver’s production of glucose by influencing enzymes involved in gluconeogenesis. In other words, it helps slow down the body’s internal glucose output, especially during periods of fasting or metabolic stress. Animal and in vitro studies have also shown cinnamon’s ability to support glycogen storage in the liver, making it easier to maintain stable energy between meals.
Some of its blood sugar benefits may also come from antioxidant and anti-inflammatory activity, which can support overall metabolic health over time.
Gut and Enzyme Effects
Cinnamon may reduce post-meal glucose spikes by slowing the digestion of carbohydrates. It has been shown to inhibit alpha-amylase, the enzyme responsible for breaking down starches in the gut. This means glucose is released more slowly into the bloodstream, preventing sharp spikes and subsequent crashes.
Lipid Metabolism
Beyond glucose regulation, cinnamon appears to positively influence cholesterol and triglyceride levels. Studies have shown reductions in total cholesterol and triglycerides, as well as modest increases in HDL. These effects may come from cinnamon’s ability to modulate lipid absorption and synthesis through changes in liver and intestinal enzyme expression.
Green Tea: Metabolic Support with Mixed Evidence
Green tea comes from the leaves of Camellia sinensis, the same plant used to produce black, oolong, and white teas. The difference lies in how the leaves are processed. Green tea is made from unfermented leaves, which helps preserve its natural green color and retain higher levels of antioxidants like polyphenols and catechins.
It’s long been recognized for its antioxidant properties, but in recent years, interest has grown around its potential role in managing blood sugar—particularly in Type 2 diabetes.
The effects of green tea on glucose regulation are thought to come from several active compounds. Tea polyphenols, caffeine, and theophylline have all been shown to influence blood sugar, insulin sensitivity, and lipid metabolism. Polyphenols in particular may help reduce blood glucose levels and improve insulin resistance, while also contributing to cardiovascular support by lowering blood lipids and slowing atherosclerosis progression.
What the Research Says
A recent meta-analysis evaluated the results of 15 randomized controlled trials studying green tea’s effects on people with Type 2 diabetes. The analysis found statistically significant improvements in several key markers:
Fasting blood glucose
HbA1c (glycated hemoglobin)
Insulin resistance index (HOMA-IR)
While these results are encouraging, the overall quality of the included studies was moderate. Only a handful used proper allocation concealment, and many excluded more recent trials due to poor data quality. Despite that, the findings still suggest a potential benefit for metabolic control with moderate green tea consumption.
Inconsistencies and Considerations
Not all studies agree. Some trials using lower doses or shorter durations didn’t find significant improvements in cholesterol, triglycerides, or HbA1c. These inconsistencies may come down to factors like:
Insufficient dosage, especially with low levels of tea polyphenols
Short study duration, which may not be enough to show long-term effects
Individual variability, including metabolic differences and how well someone absorbs or responds to tea compounds
Coexisting interventions, such as medications, dietary changes, or exercise regimens, which may mask or exaggerate results
While these results are encouraging, the overall quality of the included studies was moderate. Only a handful used proper allocation concealment, and many excluded more recent trials due to poor data quality. Despite that, the findings still suggest a potential benefit for metabolic control with moderate green tea consumption.

This is just the beginning.
In future posts, I’ll be exploring more herbs that support blood sugar balance, along with practical insight on how to actually work with them: when to use them, what forms are best, and what safety considerations matter. I also want to speak to those of us (myself included) whose blood sugar doesn’t just stay elevated but swings between highs and lows throughout the day. While much of the conversation around herbs and blood sugar focuses on lowering glucose, there’s a real need to talk about stabilizing it.
Herbal medicine isn’t a relic of the past. Many of the medications used in conventional care today were first discovered in plants, then isolated and refined in labs. But plants haven’t lost their power. They continue to offer meaningful support, especially when we understand their chemistry, their tradition, and their role in a broader system of care. In a world that often reaches for quick fixes, herbs ask us to think deeper and more holistically.
If this article resonated with you, feel free to leave a comment or share it with someone who might find it helpful. And if you're enjoying this kind of content and want to go deeper, I’d love to have you join as a paid subscriber. It’s a way to support this work and access the rest of this week’s posts, including deeper herb breakdowns, how to actually use them, and a focused post on stabilizing blood sugar with herbs.
Until next time,
-Agy | The Buffalo Herbalist
Bibliography
Hantzidiamantis, P. J., Awosika, A. O., & Lappin, S. L. (2024, April 30). Physiology, glucose. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK545201/
Cde, C. L. T. P. (2022, April 14). Examining the mechanisms of glucose regulation. AJMC. https://www.ajmc.com/view/ace005_12jan_triplitt_s4
Jia, M., Liu, X., Liang, Y., Liu, D., & Li, H. (2024). The effect of green tea on patients with type 2 diabetes mellitus: A meta-analysis. Medicine, 103(47), e39702. https://doi.org/10.1097/md.0000000000039702
Lee, J., Noh, S., Lim, S., & Kim, B. (2021). Plant extracts for Type 2 diabetes: From traditional medicine to Modern drug discovery. Antioxidants, 10(1), 81. https://doi.org/10.3390/antiox10010081
Chang, C. L. T., Lin, Y., Bartolome, A. P., Chen, Y., Chiu, S., & Yang, W. (2013). Herbal therapies for Type 2 diabetes mellitus: chemistry, biology, and potential application of selected plants and compounds. Evidence-based Complementary and Alternative Medicine, 2013, 1–33. https://doi.org/10.1155/2013/378657
Kumar, S., Mittal, A., Babu, D., & Mittal, A. (2020). Herbal Medicines for Diabetes Management and its Secondary Complications. Current Diabetes Reviews, 17(4), 437–456. https://doi.org/10.2174/1573399816666201103143225
Silva, M. L., Bernardo, M. A., Singh, J., & De Mesquita, M. F. (2022). Cinnamon as a Complementary therapeutic approach for dysglycemia and dyslipidemia control in Type 2 diabetes mellitus and its molecular Mechanism of Action: A review. Nutrients, 14(13), 2773. https://doi.org/10.3390/nu14132773
Jia, M., Liu, X., Liang, Y., Liu, D., & Li, H. (2024b). The effect of green tea on patients with type 2 diabetes mellitus: A meta-analysis. Medicine, 103(47), e39702. https://doi.org/10.1097/md.0000000000039702






Thank you so much for all of this wonderful information! ❤️
An informative read.
‘Blood sugar imbalances impact energy, mood, hormone function, inflammation, and long-term metabolic health.’
A lack of understanding, often coupled with lazy decision-making, is turning our children into gremlins in the classroom, and placing a huge burden on our already-strained healthcare systems.
Keep fighting the good fight 💪🏻