Your Gut & Brain Are Talking—Are You Listening? What Herbalists Need to Know
your gut isn’t just digesting food—it’s shaping your emotions, stress response, and cognitive function.
You know that feeling—something big is coming up. An interview, a deadline (me, yesterday!), or just the sheer terror of putting yourself out there. You’re nervous. And somehow, your gut knows it before you do.
Butterflies? Maybe. A sudden wave of nausea? Also possible. That unmistakable churning that makes you rethink all your life choices? Definitely.
But how does your stomach know? It’s not like it was in the meeting where they scheduled your presentation. It didn’t read the email reminding you that your deadline is today. And yet—there it is, reacting, tensing, flipping like it got the memo before your brain did.
What if I told you… it kind of did?
Because your gut isn’t just along for the ride—it’s in constant conversation with your brain. And sometimes, it’s the one calling the shots.
The question is: who’s really in charge—your head or your gut? Or both?
The Gut-Brain Connection: More Than Just Digestion
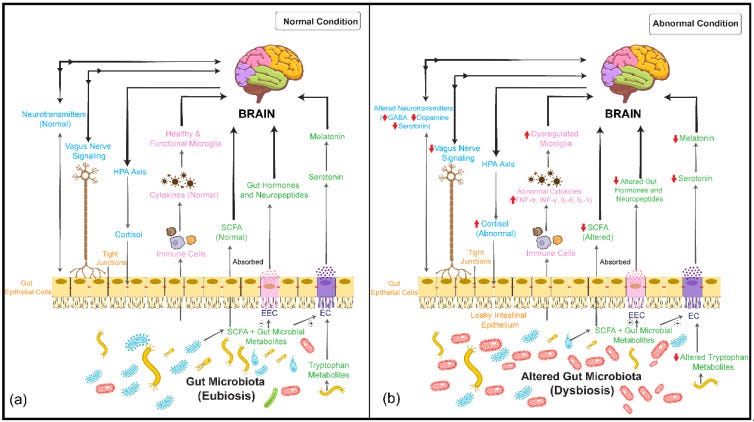
You’ve probably heard that your gut is your “second brain,” but the relationship between the gut and the brain goes far beyond digestion. This bidirectional communication system—known as the gut-brain (GB) axis—plays a crucial role in regulating everything from appetite and immune function to sleep quality.
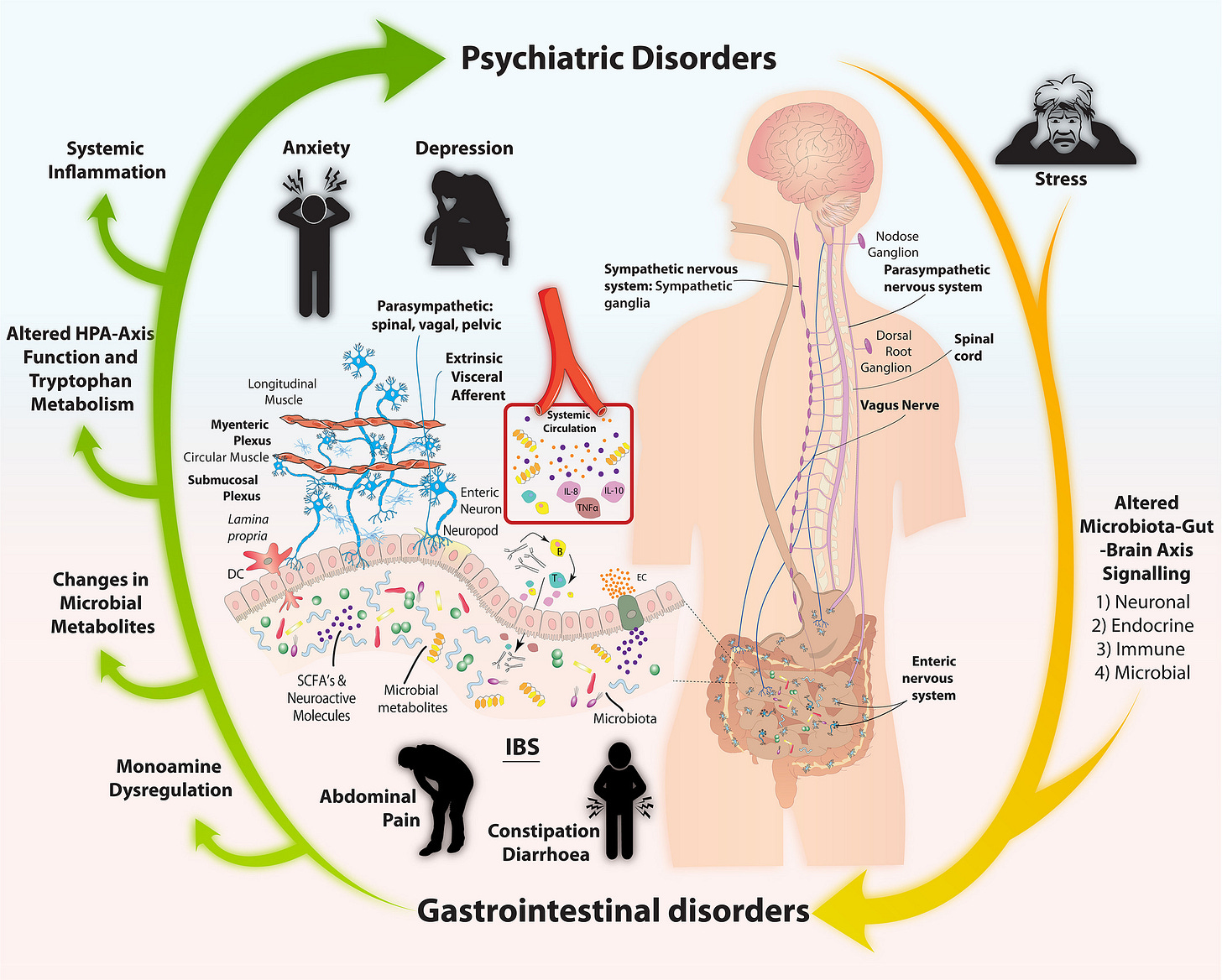
For years, researchers have suspected that imbalances in this system contribute to chronic abdominal pain and digestive disorders. In fact, what were once called functional GI disorders (like IBS and functional dyspepsia) are now officially recognized as disorders of altered gut-brain interactions. This shift in terminology reflects a deeper understanding of how these conditions arise—not just from issues in the gut, but from a complex interplay between the gut, nervous system, and even gut microbes.
Here’s where it gets even more interesting:
While there’s still debate about whether these disorders are driven more by the gut or the brain, one thing is clear—chronic abdominal pain is often linked to a dysregulated relationship between gut signals, the enteric nervous system (ENS), the central nervous system (CNS), and the gut microbiome.
Over the past 15 years, microbiome research has completely reshaped how we view the GB axis. Scientists now talk about the gut-brain-microbiome (GBM) system, which recognizes the microbiome as an active player in brain health.
And it’s not just about digestion—this research has opened doors to understanding how gut imbalances may contribute to conditions like anxiety, depression, Alzheimer’s, Parkinson’s, and even autism spectrum disorder.
The most exciting part? The gut microbiome is modifiable. That means we’re beginning to explore ways to improve both gut and brain health by supporting the microbiome—through diet, probiotics, and other interventions.(*like herbs!*)
The connection between gut health and brain function is more powerful than we once thought, and we’re only scratching the surface of how we can harness this knowledge for better health.
Your Gut Senses More Than You Think: How Interoception Shapes Your Health
Ever had butterflies in your stomach? Or felt your gut tighten with stress? That’s interoception in action—your brain’s ability to sense what’s happening inside your body. It keeps track of things like hunger, digestion, heart rate, and even emotions, helping maintain balance between your brain and gut.
For a long time, scientists thought this internal communication was handled only by nerves sending signals from the body to the brain. But recent microbiome research has flipped that idea on its head.
Turns out, your gut microbes are also key players in this process—influencing not just digestion but also mood, stress response, and even pain perception.
You’re probably wondering - how does this actually work?
Microbes send messages to your brain. Your gut bacteria produce tiny molecules (called metabolites) that can travel through the bloodstream or interact with nerve endings in your gut, sending signals straight to your brain.
These signals shape your emotions, digestion, and reflexes. Your gut and brain are constantly adjusting to keep things balanced, whether it’s regulating your appetite, controlling inflammation, or responding to stress.
Strong emotions can override this balance. Ever lost your appetite when you’re anxious? Or had an upset stomach from stress? That’s because your brain can override gut reflexes when it detects emotional or environmental threats.
Most of this communication happens through the vagus nerve, the enteric nervous system (ENS), and the gut’s immune and hormone-producing cells. When things are running smoothly, these pathways help regulate digestion, gut motility, and overall well-being. But when interoception gets disrupted—whether from chronic stress, microbiome imbalances, or inflammation—it can lead to issues like IBS, chronic abdominal pain, and even mood disorders like anxiety and depression.
A key player in all of this is the insula cortex in the brain, which processes gut signals and combines them with emotions and past experiences. When this system is out of sync, it can create a cycle where stress, pain, and gut dysfunction feed into each other.
The good news? Because the microbiome is flexible, we can support a healthier gut-brain connection through diet, lifestyle changes, and targeted interventions. Scientists are now exploring ways to fine-tune gut health to improve both digestion and mental well-being.
So next time you get a gut feeling—trust it. Your body is always talking to you. The more we understand about interoception, the better we can support our health from the inside out.
How the Gut and Brain Communicate: Breaking Down the Four Pathways
We’ve all felt it—stress hitting our stomach like a rock, anxiety twisting our gut into knots. But what if I told you that these reactions aren’t just a side effect of emotions, but part of a deeply interconnected system that scientists are still uncovering?
Research shows that the gut and brain are in constant communication, influencing everything from mood and metabolism to immune function and even behavior. As early as 1998, studies found that simply introducing Campylobacter jejuni (a common gut bacterium) into rats—without triggering an immune response—caused them to show signs of anxiety. Later studies confirmed that this effect was linked to signals traveling from the gut to specific regions of the brain, all through the vagus nerve.
So, how does this gut-brain dialogue actually work?
Scientists have identified four major pathways through which the gut microbiome influences the brain: neurologic, endocrine, humoral/metabolic, and immune pathways. Let’s break them down.
1. The Neurologic Pathway: The Gut’s Direct Line to the Brain
The gut has its own nervous system—the enteric nervous system (ENS)—which constantly sends messages to the brain via the vagus nerve. This pathway is a powerhouse of neurotransmitters, producing GABA, serotonin, melatonin, histamine, and acetylcholine—all of which influence mood, sleep, and digestion. In fact, the gut makes about 95% of the body’s serotonin, the same neurotransmitter targeted by many antidepressants.
Beyond neurotransmitters, the autonomic nervous system also plays a role in gut health by regulating immune responses—modulating how gut macrophages and mast cells respond to bacteria. Disruptions in this system can lead to imbalances in gut motility, inflammation, and even heightened pain sensitivity.
2. The Endocrine Pathway: Hormones and the Stress Response
The gut microbiome plays a key role in nutrient absorption, which in turn affects the release of hormones from enteroendocrine cells—specialized cells that communicate with the brain. One major player is galanin, a neuropeptide involved in everything from appetite and sleep to mood and stress regulation. Galanin activates the HPA axis, a major stress response system that controls cortisol production. This means gut imbalances can directly impact how the body handles stress—potentially contributing to anxiety, mood swings, and even chronic fatigue.
3. The Humoral/Metabolic Pathway: Microbial Metabolites and Brain Function
One of the most fascinating areas of gut-brain research involves short-chain fatty acids (SCFAs)—molecules produced when gut bacteria ferment dietary fiber. These SCFAs aren’t just fuel for gut cells; they also have hormone-like effects, influencing inflammation, metabolism, and even nerve function.
SCFAs can cross the blood-brain barrier, where they help regulate brain immune cells (microglia), which are critical for brain development and emotional regulation. Interestingly, disruptions in SCFA metabolism have been linked to autism spectrum disorder (ASD)—with research suggesting that imbalances in gut bacteria could alter brain signaling and social behavior.
Another major microbial byproduct is lipopolysaccharide (LPS), a component of bacterial cell walls. When the gut barrier is compromised (often referred to as "leaky gut"), LPS can enter the bloodstream, triggering widespread inflammation. Studies have found that people with depression tend to have higher levels of LPS antibodies, suggesting a direct link between gut inflammation and mental health.
4. The Immune Pathway: How the Microbiome Shapes Inflammation
The gut microbiome is deeply intertwined with the immune system, influencing the release of cytokines (immune signaling molecules) that can either promote or reduce inflammation. In conditions like IBS, gut dysbiosis (an imbalance in microbiota) has been shown to activate immune responses that increase gut permeability, leading to chronic inflammation, visceral hypersensitivity (heightened gut pain), and altered gut motility.
This immune-gut connection also explains why stress, diet, and microbiome imbalances can trigger both digestive issues and mood disturbances—because when gut inflammation spikes, it can send distress signals to the brain, disrupting emotional regulation and even contributing to disorders like anxiety and depression.
So, why does this even matter?
The more we learn about the gut-brain axis, the clearer it becomes: mental and gut health are inseparable.
Our microbiome isn’t just digesting food—it’s producing neurotransmitters, modulating hormones, influencing stress responses, and even shaping our immune system.
If you’ve ever wondered why stress wrecks your digestion, or why gut health seems to play a role in mood disorders, this is why.
And the best part? Since the microbiome is constantly adapting, we have the power to support this system—through diet, stress management, and targeted interventions that promote a healthier gut and a healthier mind.
Your gut isn’t just talking to your brain—it’s shaping your entire experience of the world. Maybe it’s time we started listening.
Herbs, the Gut, and Mental Health
While modern medicine often focuses on pharmaceuticals for mental health, the plant world has been offering its own solutions for centuries. Some medicinal herbs don’t just influence mood—they also have a direct impact on the gut microbiome, which, as we now know, plays a major role in mental well-being.
Let’s look at three powerful herbs that support both the gut and the mind.
St. John’s Wort (Hypericum perforatum) – The Herbal Antidepressant
One of the most well-researched herbal remedies for depression, St. John’s Wort has been shown in numerous studies to be as effective as selective serotonin reuptake inhibitors (SSRIs) for mild to moderate depression, with fewer side effects and a lower risk of discontinuation.
Its antidepressant effects come from a mix of active compounds, including hyperforins, flavonoids (like hyperoside), hypericin, and procyanidins. But here’s where it gets even more interesting—St. John’s Wort doesn’t just affect brain chemistry.
A recent study found that in ovariectomized rats (a model for estrogen deficiency), St. John’s Wort extract helped restore gut microbiome balance, reversing changes in the Firmicutes/Bacteroidetes ratio—a key marker in gut health. This suggests that part of its antidepressant power may come from its ability to influence gut bacteria.
Just remember: St. John’s Wort interacts with a lot of medication (read more about that here: Herbal Safety: What Every Beginner Should Know)
As always – with any and all herbal info I give – consult with your healthcare provider and do your own research!
Rhodiola (Rhodiola rosea) – The Adaptogen for Stress & Mood
If you’ve ever looked into herbal remedies for stress, fatigue, or anxiety, you’ve probably come across Rhodiola rosea. Used in traditional medicine for centuries, Rhodiola is a well-known adaptogen, meaning it helps the body adapt to stress while also supporting cognitive function and mood.
Rhodiola’s benefits come from its rich mix of phenolic compounds, including catechins, procyanidins, and salidroside. But its effects don’t stop at neurotransmitters—it also shapes the gut microbiome.
Studies in fruit flies (Drosophila melanogaster) showed that Rhodiola extract significantly altered gut microbiota, reducing Lactobacillales and increasing Acetobacter levels. In human fecal studies, metabolites like cinnamyl alcohol, tyrosol, and hydroquinone were identified—compounds that have been linked to neuroprotective effects, improved cognitive function, and brain resilience.
Tyrosol can cross the blood-brain barrier and has been shown to protect and regenerate neurons.
Hydroquinone has demonstrated protective effects against brain ischemia, hinting at Rhodiola’s potential in long-term brain health.
By michael clarke stuff - Flower yellow, CC BY-SA 2.0,
Cannabis (Cannabis sativa) – The Gut-Brain Regulator
While best known for its use in pain management, nausea relief, and sleep support, Cannabis sativa has some fascinating gut-brain interactions as well.
Its primary active compounds, tetrahydrocannabinol (THC) and cannabidiol (CBD), act on the endocannabinoid system, which plays a direct role in gut motility, digestion, and microbiome composition. However, these effects depend on the specific cannabinoid ratio in a given strain or extract.
In a study examining how cannabis extracts influenced gut bacteria in mice on a high-fat/cholesterol diet (HFCD):
A CBD-rich extract improved the gut microbiome by increasing the Bacteroidetes/Firmicutes ratio! We already know this tells us we have good gut health!
THC-rich and balanced THC/CBD extracts, however, did not significantly alter the microbiome.
This suggests that CBD may be the key player when it comes to gut-brain benefits, potentially helping regulate microbiome balance in conditions influenced by inflammation and metabolic dysfunction.
What I Want You to Takeaway
All of this brings us to one key takeaway: mental health isn’t just about the brain—it’s about the whole system. The gut and brain are in constant conversation, and what happens in one inevitably affects the other. The foods we eat, the microbes we nurture, and the herbs we use don’t just support digestion—they influence mood, cognition, and even resilience to stress.
So, if we truly want to support mental well-being, we have to start thinking holistically. Instead of separating gut health and brain health, maybe it’s time we start seeing them for what they really are—two parts of the same intricate, beautifully connected system.
What if the missing piece in your mental health toolkit isn’t just in your head, but in your gut?

If this article resonated with you, like, comment, and restack—it helps this information reach more people who might need it!
Coming up Friday for The Buffalo Herbalist Community: We’re diving deeper into the specific mechanisms behind how gut bacteria influence herbal medicine, key insights for herbalists, and, of course—more herbs!
If you’d like to support this publication and access The Buffalo Community articles and study materials, consider upgrading to paid. Your support keeps this space thriving and allows me to continue creating in-depth, research-backed herbal content.
See you Friday!
-Agy
Bibliography:
Pferschy-Wenzig, E., Pausan, M. R., Ardjomand-Woelkart, K., Röck, S., Ammar, R. M., Kelber, O., Moissl-Eichinger, C., & Bauer, R. (2022). Medicinal plants and their impact on the gut microbiome in mental health: A systematic review. Nutrients, 14(10), 2111. https://doi.org/10.3390/nu14102111
Images & text:
Mayer, E. A., Nance, K., & Chen, S. (2021). The gut–brain axis. Annual Review of Medicine, 73(1), 439–453. https://doi.org/10.1146/annurev-med-042320-014032






Again, this ties directly into what we are working on for ourselves based on what I deciphered in Tom's lab reports. I don't know if it will make a huge difference for me in terms of my autism, but I'm hoping to at least get some relief from my physical issues.
Top tier piece. 👌