The Gut’s Secret Guardians: How Your Immune System and Microbiome Work Together
from peyer’s patches to astragalus—exploring the hidden connections between gut health, immunity, and herbal support
Happy First Day of Spring, my friends!
We made it. I swear every cell in my body is acting like a sunflower today, stretching toward the Sun. And Buffalo? Shockingly warm—76°F. CRAZY. Definitely not complaining, though. I’ll be spending the day finishing this article, heading to the barn for a ride, and soaking up some much-needed Vitamin D.
And since the first day of Spring feels like a fresh start, and what better way to celebrate than with 10% off an annual membership to The Buffalo Herbalist Community? If you’ve been thinking about joining, now’s the perfect time—but don’t sleep on it! This deal is only available until March 21st.
What does this mean for you? Instead of paying $7/month ($84 total for the year), or the usual $77/year, you’ll get an annual membership for just $69.30—saving you up to $14.70 if you’ve been subscribing monthly or $7.70 off the yearly rate.
This gets you exclusive deep dives, case studies, materia medicas, research-backed herbal knowledge, and soon—printable PDFs for easy reference.
Click below to lock in this deal before it’s gone! 🌿✨
[Get The Spring Discount Here!]

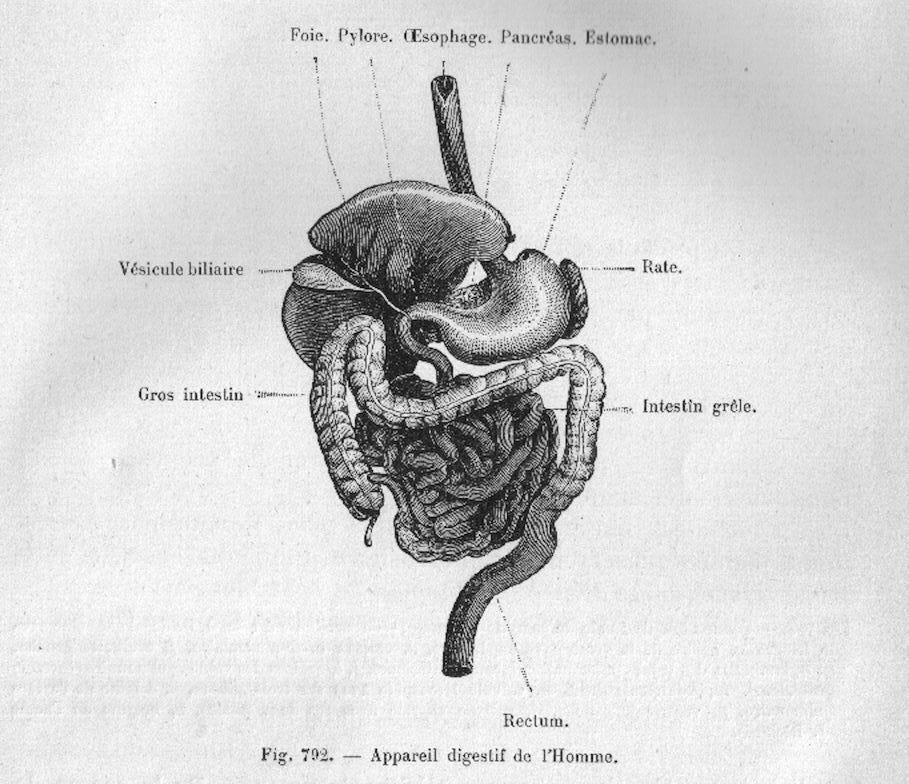
Now, onto today’s topic—one that I find not only incredibly interesting but also a bit under-discussed in herbalism. Gut health has been having its moment in mainstream wellness (which is great!), but the term itself? A little vague. We hear a lot about SIBO, chronic gut inflammation, pre- and probiotics, and all the usual suspects. But what I’ve noticed is that much of the conversation skims over the actual physiology and pathophysiology behind it all.
So, my goal for today’s article (and Friday’s) is to break that down for you—without making it overly complicated—while also highlighting some incredible herbs that can support gut health.
We’re focusing on the Gut-Lymph Connection, which, of course, also ties into the Gut-Immune Connection (because nothing in the body works in isolation, right?). If you caught the Lymphatic System article and lecture, you’ll remember that the lymphatic system and immune system are deeply intertwined
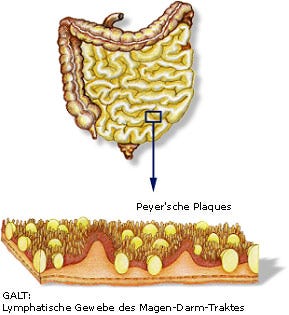
Refresher: The lymphatic system isn’t just about drainage—it’s one of the body’s main immune hubs, constantly scanning for invaders and moving white blood cells where they’re needed. And since about 70% of immune activity happens in the gut (shoutout to GALT), it makes sense that the lymph, immune, and digestive systems are all working together behind the scenes.
With that in mind, let’s take a closer look at the gut—because if the lymphatic system is the body’s surveillance network, then the gut is its command center, constantly communicating with the immune system and beyond.
Your gut is constantly sensing, reacting, and adapting—it’s not just breaking down food, it’s managing immune responses and nervous system signals in real-time. But when something throws that balance off—whether it’s an infection, food intolerance, or a flood of bacterial byproducts—the immune system picks up on it immediately and launches a full-blown inflammatory response.
This sets off a chain reaction: inflammatory mediators flood the gut, triggering increased motility, excessive secretions, and—you guessed it—diarrhea. It’s not just your body freaking out; it’s a coordinated defense mechanism designed to flush out whatever’s irritating the system.
But here’s where it gets even more interesting: your enteric nervous system (aka your "second brain") is deeply involved in this process. It doesn’t just regulate digestion—it helps maintain gut barrier integrity, modulates immune responses, and directly reacts to inflammation. Chronic gut inflammation can actually rewire gut nerve function over time, making the digestive system more sensitive and reactive.
This gut-immune-nervous system connection is central to understanding functional gut disorders. It explains why symptoms aren’t just about digestion—they’re about immune signaling, nervous system dysregulation, and gut barrier integrity all working (or not working) together.
The Gut & Immune System: A Delicate Balance
Your gut is home to a mind-blowing 40 trillion microorganisms, all working behind the scenes to keep you healthy. But they’re doing way more than just breaking down food—your gut microbiota helps regulate immune function, prevent pathogen overgrowth, metabolize complex carbohydrates, and even detoxify bile acids. It’s a full-scale immune and metabolic machine.
But here’s where things get even more interesting: the gut isn’t just teeming with microbes—it’s also one of the most immune-active regions in the entire body. The immune system has to constantly assess and respond to what’s coming through—deciding whether to tolerate a harmless microbe, neutralize a potential threat, or launch a full-blown inflammatory response.
When everything is in balance, this system works beautifully—harmful bacteria get eliminated while beneficial microbes thrive. But when this balance is disrupted, the immune system overreacts—leading to conditions like Crohn’s disease, ulcerative colitis, irritable bowel syndrome, and chronic inflammation.
Because the gut plays such a huge role in immune function, it contains the highest concentration of immune cells in the body. These immune hubs fall into two main categories:
Inductive sites – The training ground for adaptive immune cells, including the mesenteric lymph nodes (MLN) and gut-associated lymphoid tissues (GALT).
Effector sites – The frontline defense, where activated immune cells work to maintain gut barrier integrity (think of the intestinal lamina propria and epithelium).
The Role of Gut-Associated Lymphoid Tissue (GALT)
One of the biggest players in gut immunity is the gut-associated lymphoid tissue (GALT)—a widespread network of immune tissues that acts as a bridge between the gut and the immune system.
Unlike other immune tissues, GALT is in a constant state of activation because the gut is always exposed to new antigens from food, microbes, and environmental factors. This means it has a unique job—tolerate beneficial bacteria and food particles while staying ready to attack harmful invaders.
One of GALT’s most important functions is training B cells, the immune cells responsible for producing antibodies. Interestingly, many of the antibody-producing B cells in GALT mature independently of T cells, meaning the gut has its own specialized way of developing immune defenses.
B cells trained in GALT help produce IgA antibodies, which are critical for maintaining gut balance.
These antibodies specifically target glycans (complex sugars) commonly found on microbiota species, suggesting an evolutionary adaptation to maintaining gut homeostasis.
In simple terms? Your gut is shaping your immune system daily.
Why does GALT Matter
Unlike other lymphoid tissues, GALT isn’t just reacting to pathogens—it’s actively shaping long-term immune function. It teaches the immune system what to tolerate, what to fight, and how to maintain a healthy balance.
New research suggests that GALT plays a major role in B cell diversification, meaning its impact on immunity extends far beyond the gut.
So, what does this mean for you?
When the gut is healthy, your immune system is balanced, inflammation stays in check, and your body runs smoothly.
When gut balance is disrupted, immune function can go rogue—leading to chronic inflammation, food sensitivities, and autoimmune issues.
We’re learning more every day about the gut-immune connection, and it’s reshaping how we understand autoimmune conditions, chronic inflammation, and even systemic immunity. And at the root of it all? The health of your gut.
Peyer’s Patches: The Gut’s Immune Watchtower
Again, your gut isn’t just digesting food—it’s on constant surveillance. And at the frontlines of this immune intelligence? Peyer’s Patches.
These small but mighty immune hubs are embedded throughout the intestinal lining, acting like border control agents, scanning everything that comes through. Their job? Distinguish between friend and foe—deciding whether to let a microbe pass peacefully or sound the alarm for an immune response.
Peyer’s Patches were first described way back in 1677, but we’re still uncovering just how important they are in gut health, immunity, and even autoimmune conditions.
How Peyer’s Patches Work
Each Peyer’s Patch is a tightly packed cluster of immune cells, surrounded by a specialized epithelium full of M cells—tiny sentinels that grab bacteria, viruses, and antigens from the gut and hand them off to immune cells below.
Once this happens, the immune system makes a call:
✔ Tolerate it (if it’s a beneficial microbe that helps gut function)
✔ Attack it (if it’s a pathogen trying to cause chaos)
This balance is critical—because the gut isn’t just a passive tube for digestion. It’s one of the most immune-active organs in the body, constantly deciding whether to keep the peace or go to war.
Peyer’s Patches & Pathogens: A Double-Edged Sword
Peyer’s Patches are designed to detect threats, but some pathogens have figured out how to exploit them.
Bacteria like Salmonella, E. coli, and Yersinia use Peyer’s Patches as a shortcut—bypassing normal gut defenses to invade deeper tissues. Some, like Listeria monocytogenes, hijack these immune hubs to spread quickly through the body.
And it’s not just bacteria—viruses, including Poliovirus, HIV, and Reovirus, also use Peyer’s Patches as an entry point into the body. In some cases, like prion diseases, these patches even become a pathway for neurodegenerative conditions.
So while Peyer’s Patches are essential for gut defense, they can also become an Achilles' heel when pathogens take advantage of them.
Peyer’s Patches & the Gut-Immune Connection
Beyond just defending against infections, Peyer’s Patches actively shape long-term immune function. They regulate T-cell responses, help produce IgA antibodies, and work closely with gut microbiota to maintain immune balance.
When they’re functioning well? They help prevent unnecessary inflammation and train the immune system to recognize what’s truly harmful.
When things go sideways? They can trigger chronic inflammation—leading to conditions like Crohn’s disease and Graft-versus-Host Disease (GVHD).
Mutations in NOD2, a key immune receptor found in Peyer’s Patches, have even been linked to Crohn’s disease, further proving how critical these immune hubs are in maintaining gut health.
Give To Me Straight
Peyer’s Patches are not just some obscure anatomical feature—they’re an essential interface between the gut and immune system.
They decide what gets tolerated and what gets attacked.
They influence autoimmune conditions like Crohn’s disease.
They help train the immune system to react appropriately to gut bacteria.
Understanding how they work helps us see why gut health is so much bigger than just digestion—it’s a key player in immune regulation, chronic disease prevention, and overall resilience.
The Gut Barrier: Your Body’s First Line of Defense
Peyer’s Patches are constantly sampling what passes through the gut, deciding whether to activate an immune response or let things slide. But they’re not working alone—the gut lining itself plays a crucial role in deciding what gets absorbed and what stays out.
The gut wall isn’t just some passive lining—it’s an intelligent, highly selective barrier designed to absorb nutrients while blocking bacteria, toxins, and other harmful substances from slipping into circulation.
But when the gut barrier becomes compromised, things start slipping through that shouldn’t be in circulation. This is known as increased intestinal permeability (often called “leaky gut”), and it’s linked to everything from chronic inflammation to autoimmune disease.
Certain medications, like NSAIDs, can damage enterocyte mitochondria (aka the energy powerhouses of gut lining cells), making the barrier more vulnerable to bacterial infiltration and immune activation.
Untreated Crohn’s disease increases gut permeability, allowing larger molecules to cross into tissues and provoke a chronic inflammatory response. Interestingly, when Crohn’s patients switch to an elemental diet (a highly absorbable, pre-digested diet used in treatment), permeability decreases—right alongside symptoms.
Even kidney disease has been linked to gut permeability, with studies showing a correlation between intestinal barrier dysfunction and elevated IgA (a key immune marker in the blood).
A dysfunctional gut barrier isn’t just a gut issue—it’s an immune system issue. When the gut lining becomes too permeable, the lymphatic system is the next line of defense, picking up inflammatory waste, bacterial byproducts, and excess immune cells. And if the lymphatic system gets overwhelmed? That’s when we see systemic stagnation, chronic inflammation, and immune dysregulation.
Astragalus & Gut Health: More Than Just an Immune Herb
An herb I want to reintroduce you to is Astragalus—and why reintroduce? Because while it’s typically known for its immunomodulating properties and adaptogenic effects, recent research is showing that its impact on gut health is absolutely wild. Beyond immune support, Astragalus plays a major role in strengthening the intestinal barrier, balancing the microbiome, and reducing gut-driven inflammation.

How Astragalus Supports the Gut, Lymph, and Immune System
Saponins (like Astragaloside IV) help modulate the gut microbiota by increasing beneficial short-chain fatty acids (SCFAs) like butyrate, which supports the gut lining and reduces inflammation. They also reduce oxidative stress, lower insulin resistance, and help maintain pancreatic and liver health, which indirectly benefits gut function.
Polysaccharides in Astragalus have a profound impact on the microbiome, increasing beneficial bacteria like Lactobacillus and Akkermansia while suppressing harmful strains. They also help regulate blood sugar, reduce intestinal inflammation, and strengthen gut barrier integrity by reducing oxidative stress and protecting against intestinal permeability.
Flavonoids contribute to gut barrier repair by enhancing tight junction integrity, reducing systemic inflammation, and lowering oxidative stress. These compounds have also been shown to support glucose metabolism, lower cholesterol, and regulate bile acid production—all of which play a role in gut-liver function.
Astragalus & the Gut Barrier
One of the most exciting aspects of Astragalus is its role in protecting and repairing the gut barrier. Studies suggest that its polysaccharides and flavonoids help strengthen epithelial tight junctions, preventing unwanted substances from leaking into circulation and triggering inflammation. This has important implications for leaky gut, autoimmune conditions, and metabolic disorders.
Beyond gut health, these effects extend to the lymphatic and immune systems—since a compromised gut barrier means more inflammatory waste and immune activation, Astragalus’ ability to regulate microbiome balance, reduce gut inflammation, and fortify barrier integrity makes it a powerhouse herb for immune resilience.
Don’t forget—the Spring Equinox discount ends soon! If you’ve been enjoying these posts and want to go deeper into herbalism, formulation, and clinical insights, this is the perfect time to join the Buffalo Herbalist Community at 10% off for the whole year (forever!)
This membership isn’t just about more content—it’s about building an herbal study resource you can return to again and again. I’m also working on printable PDFs for easy note-taking and materia medicas of the herbs we’ve covered—so you can start building your own herbal study binder!
And don’t miss Friday’s post—we’re going even deeper into the pathophysiology of gut-immune interactions and introducing new herbs that support the gut and lymphatic system. 🌿
⏳ The 10% off deal disappears after March 21st! Lock in your spot here:
[Get The Spring Discount Here!]

If you found this post helpful, feel free to like, comment, share, or restack so more people can join the conversation.
I always love hearing your thoughts, insights, and experiences, so don’t hesitate to drop a comment.
Your support helps keep this community growing, and I truly appreciate every one of you who takes the time to read, engage, and learn alongside me.
Wishing you a season of fresh starts, warm sunlight, and plenty of time to steep in all the good things—herbal and otherwise.
See you Friday!
- Agy
Bibliography
Bemark, M., Pitcher, M. J., Dionisi, C., & Spencer, J. (2024). Gut-associated lymphoid tissue: a microbiota-driven hub of B cell immunity. Trends in Immunology, 45(3), 211–223. https://doi.org/10.1016/j.it.2024.01.006
Jung, C., Hugot, J., & Barreau, F. (2010). Peyer’s patches: the immune sensors of the intestine. International Journal of Inflammation, 2010, 1–12. https://doi.org/10.4061/2010/823710
Mörbe, U. M., Jørgensen, P. B., Fenton, T. M., Von Burg, N., Riis, L. B., Spencer, J., & Agace, W. W. (2021). Human gut-associated lymphoid tissues (GALT); diversity, structure, and function. Mucosal Immunology, 14(4), 793–802. https://doi.org/10.1038/s41385-021-00389-4
Su, M., Tang, T., Tang, W., Long, Y., Wang, L., & Liu, M. (2023). Astragalus improves intestinal barrier function and immunity by acting on intestinal microbiota to treat T2DM: a research review. Frontiers in Immunology, 14. https://doi.org/10.3389/fimmu.2023.1243834




I love this article. If anyone is looking for an easy way to incorporate astragalus into their diet, I usually put it in a reusable teabag and brew it with any stock I am making. Then I just use the stock in everything. 💚
Thank you so much for this article! I have IBD and the autoimmune disorder, psoriasis with psoriatic arthritis. I've done all kinds of research to help my gutt heal which consequently heals my skin and joints. But i hadn't tried astragalus. Currently self treating with Mediterranean diet, slippery elm bark capsules and turmeric capsules... well and many many herbal tea blends (growing a medicinal herb garden). I also noticed that getting my nervous system out of the constant fight or flight mode by giving in and getting PTSD in check has helped both too!